The elderly population is growing, and individuals aged 65 and over will increase from 13% of the US population in 2010 to 20% by 2030. Geriatric patients undergo a large proportion of operative procedures and have increased complications, morbidity, and mortality, which may be associated with increased intensive care unit (ICU) time, length of stay, and hospital readmission (1). With the expanding elderly population, identification of optimal anesthesia care for geriatric patients will have outsized value for individual patients and society.
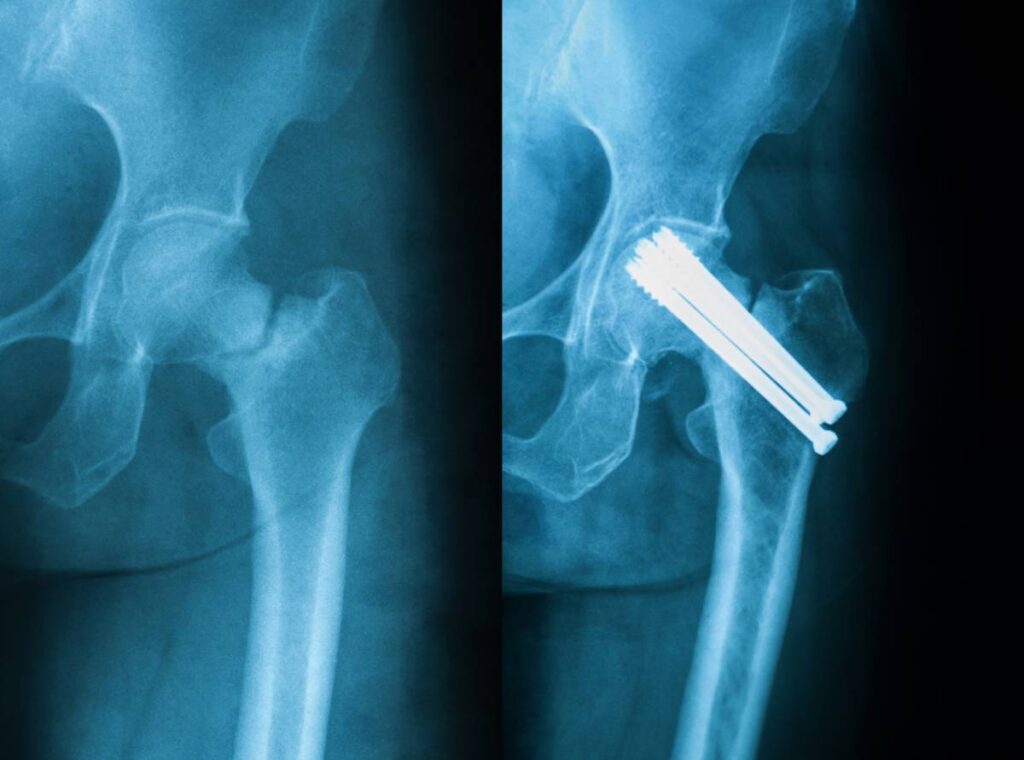
Fragility fractures—hip fractures in elderly patients from low-impact falls associated with osteoporosis—are the second most common reason for hospital admission in elderly patients and account for significant morbidity, mortality, and cost (1). In general, the patient with a hip fracture presents to the emergency department for evaluation and stabilization before proceeding to the inpatient ward or operating room. A focused history, physical, and review of prior evaluations is prudent before going to the operating room, especially if the cause of the fall is not established. Delay in time to operation is a risk factor for poor perioperative outcomes in the geriatric patient and has been associated with worse outcomes, increased duration of stay, and decubitus ulcers (1). Therefore, it is important to minimize delay to surgery for patients who are optimized for the operating room.
Although it remains controversial, the majority of studies comparing regional versus general anesthesia suggest that regional anesthesia may be superior in major orthopedic surgery. In 2012, Neuman and colleagues retrospectively analyzed the records of more than 18,000 patients undergoing surgery for hip fracture and found regional anesthesia associated with a 25% to 29% decrease in major pulmonary events and mortality (2). Similarly, Memtsoudis and colleagues evaluated data from 382,236 records and showed a decreased major morbidity and mortality rate associated with regional anesthesia for patients undergoing total knee arthroplasty and a trend toward lesser major morbidity and mortality for total hip arthroplasty. Regional anesthesia is usually administered with sedation, but few studies comparing general anesthesia and regional anesthesia have focused on depth of anesthesia and sedation.
Recently, Sieber and colleagues conducted a randomized trial of light sedation (Bispectral Index of ∼50) versus deep sedation (Bispectral Index >80) in geriatric patients undergoing hip fracture repair under spinal anesthesia. They found a 50% reduction in the incidence of delirium in the light sedation group. In a follow-up survival analysis, Brown and colleagues found that, in patients with serious comorbidities, mortality was significantly reduced at 1 year in the light sedation group (3). These findings suggest that, in the highest risk geriatric patients, regional anesthesia with light sedation may be superior to regional anesthesia with deep sedation, although further research is needed.
Patients with hip long bone fractures are at high risk for deep vein thrombosis and prophylaxis should be initiated preoperatively and continued through the intraoperative and postoperative course to prevent deep vein thrombosis and pulmonary embolism. Additionally, prevention of pressure ulcers can begin in the perioperative period and can reduce morbidity significantly and improve outcomes (1). Increasingly, goals of care after fixation of hip fracture are early mobilization and rehabilitation. Rapid recovery from anesthesia and sedation while maintaining adequate pain control is important, and can be obtained with patient-controlled analgesia.
References
1. Lester L. Anesthetic Considerations for Common Procedures in Geriatric Patients: Hip Fracture, Emergency General Surgery, and Transcatheter Aortic Valve Replacement. Anesthesiol Clin. 2015;33(3):491-503. doi:10.1016/j.anclin.2015.05.006
2. Neuman MD, Silber JH, Elkassabany NM, Ludwig JM, Fleisher LA. Comparative effectiveness of regional versus general anesthesia for hip fracture surgery in adults. Anesthesiology. 2012;117(1):72-92. doi:10.1097/ALN.0b013e3182545e7c
3. Brown CH 4th, Azman AS, Gottschalk A, Mears SC, Sieber FE. Sedation depth during spinal anesthesia and survival in elderly patients undergoing hip fracture repair. Anesth Analg. 2014;118(5):977-980. doi:10.1213/ANE.0000000000000157